Tularemia also found in hares in Gelderland
Tularemia in hares
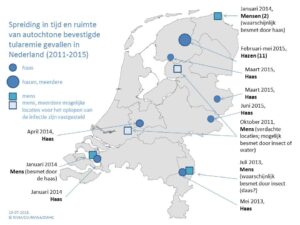
Tularemia has been identified in a hare from the Dutch province of Gelderland that was submitted to the Dutch Wildlife Health Centre (DWHC) in June 2015 for post-mortem exam. Since 2011, all dead hares received by the DWHC are routinely tested by the Central Veterinary Institute for the bacteria that causes Tularemia (Francisella tularensis). The map shows all reported cases of tularemia in people and hares since 2011; in most of the provinces the disease has been only sporadically reported but in 2015 in one area of Friesland, 11 cases have been documented in hares with three individual cases occurring in another part of Friesland, Gelderland and Overijssel. In 2014 the disease was diagnosed in two people in the northerly province of Groningen bringing the total number of affected provinces to seven.
© RIVM/CVI/NVWA/DWHC
Signs in animals
Hares with tularemia are typically weak, apathetic and unsteady on their feet. They may show a reduced flight response and allow themselves to be caught. Tularemia in wild animals is not treated.
Tularemia in people
Tularemia in humans is very rare. People can become infected via contact with animals (in particular hares and rodents) but the bacteria is not transmitted from person to person. The most common routes of infection include:
- Via the skin e.g. small wounds or insect bites
- Ingestion of insufficiently cooked infected meat; the bacteria can be killed by heating to at least 60°C.
- Consumption of contaminated surface water
Symptoms in people
The nature of clinical signs depends on the route and source of infection. For example, infection via the skin typically leads to the development of an ulcer a few days later often accompanied by swelling of the regional lymph node (i.e. lymph nodes in the elbow or armpit of the affected arm/hand, or in the groin of the affected leg). Infection may be accompanied by fever and flu-like signs. It is usually treatable with appropriate antibiotics.
Contact your doctor if you become sick after handling dead hares or rodents and inform the doctor of the nature of this contact. More information about infection in people is available from the website of the Centres for Disease Control.
Tularemia in dogs and cats
Pets and other animals that come into contact with or eat infected hares can become infected with F. tularensis. In the Netherlands mild illness was seen in a dog that had licked up blood from an infected hare. In general dogs are much less sensitive to infection with this bacteria and if they do become infected signs are typically mild and may include reduced appetite, fever and general malaise. These signs are not exclusive to infection with F. tularensis and if your dog does become ill after contact with infected animals seek advice from your vet. Blood tests for F. tularensis can be performed at the Central Veterinary Institute in Lelystad. Whilst there are descriptions of cats in the USA becoming infected with F. tularensis and showing anorexia, vomiting and weight loss, this has not yet been reported amongst cats that have come into contact with infected hares in the Netherlands. A different sort of F. tularensis causes tularemia in the USA and it is unknown as to whether and to what extent the sort seen in Europe poses a risk to cats.
Preventative measures
In the countryside protect yourself from biting insects with products or appropriate clothing. Gloves should always be worn when handling animal carcasses and wounds should be thoroughly disinfected and covered.
Reporting a dead hare
You can report finding one or more dead hares (or other animals) in the wild, via the submission form on our website. After submitting your form you will be contacted by the DWHC who will help to decide whether or not further investigation is necessary and will advise you on how to package the cadaver and arrange collection of the package from your home or place of work.



